🧬 Lyme Disease 101 | The Ultimate Guide
🧩 Understanding Lyme Disease: A Comprehensive Guide
Lyme disease is a complex and often misunderstood illness that can deeply affect a person’s health and quality of life. Caused by a type of bacteria transmitted through tick bites, it’s often called “the great imitator” because its symptoms can mimic those of many other conditions. However, with the right information, you can gain a clearer understanding of the disease, recognize the signs, and take meaningful steps toward effective treatment and recovery. This guide provides a solid foundation of knowledge to help you in your journey.
And, if you’re feeling overwhelmed or like you’ve tried everything, please remember: you’re not alone. Our goal is to provide a comprehensive resourcec that may include insights, strategies, and approaches you haven’t explored before.
📘 What is Lyme Disease?
Lyme disease, also known as Lyme borreliosis, is an infectious illness caused by the bacterium Borrelia burgdorferi (and related species). It is most commonly transmitted to humans through the bite of an infected black‑legged tick (deer tick), but can be contracted in many other ways. Ticks acquire the bacteria by feeding on infected animals.
The disease was first recognized in 1975 in the town of Lyme, Connecticut, when a group of children developed unusual arthritis‑like symptoms. In 1981, Dr. William Burgdorfer, a researcher at the National Institute for Allergy and Infectious Diseases (NIAID), identified the spiral‑shaped bacteria -known as spirochetes- responsible for the illness. The organism was later named Borrelia burgdorferi in his honor. Since then, more than 6,000 scientific studies have explored the clinical, epidemiological, and microbiological aspects of Lyme disease.
Lyme disease can affect multiple systems in the body, including the skin, joints, nervous system, brain, and heart.
The symptoms of Lyme disease can vary widely and may include:
- A characteristic skin rash known as erythema migrans (bull’s‑eye rash)
- Fever and chills
- Fatigue
- Headaches and migraines
- Muscle and joint pain
- Swollen lymph nodes
- And potentially hundreds of other symptoms
If left untreated, Lyme disease can progress and cause more severe complications such as chronic arthritis, heart rhythm disturbances, neurological issues, and in rare cases, even death.
Early detection and diagnosis is critical — prompt diagnosis and treatment, usually with antibiotics, offer the best chance to prevent long‑term health problems.
Scroll down to learn more about treatment options, prevention strategies, and ways to manage Lyme disease and its co‑infections.
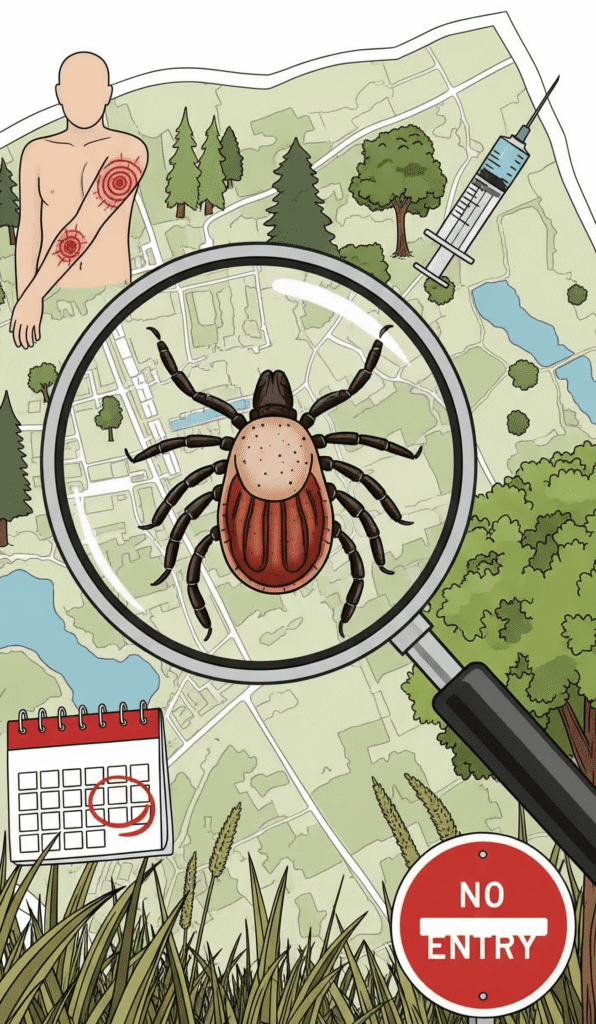
⚠️ How do you get Lyme disease?
Lyme disease bacteria, borrelia burgdorferi, is most often spread to humans through the bite of an infected tick or infected biting insect.
Lyme disease can also be contracted via other methods such as:
- Other insect bites (there is some evidence that other insects like mosquitoes, fleas, and lice may also be able to transmit the bacteria that cause Lyme disease, although this mode of transmission is thought to be less common than tick bites),
- Mother-to-child (Transmission may occur through the placenta during pregnancy or possibly bia breast milk),
- Exposure to contaminated blood, and
- Possibly even sexually transmitted (studies are still in progress to confirm or deny).
It’s important to note that not every tick or insect carries Lyme bacteria, and not every bite will lead to infection. However, awareness of all possible transmission routes can help in early recognition, testing, and prevention.
🤒 Lyme Disease Symptoms
The symptoms of Lyme disease are highly varied and can manifest at different times after infection, often progress through distinct pages. It is important to understand that not all individual will experience every symptom, and the way the disease unfolds can vary slightly from one person to another, making it a challenging condition to track and diagnose.
This stage is sometimes marked by the most well-known sign of Lyme: the erythema migrans (EM) rash. Oftend described as a bull’s eye, this rash can be solid red or appear in other shapes. It’s important to know that many people do not get this classic rash.
Other symptoms at this stage may include:
- Fever, chills, and sweats
- Fatigue, malaise, and a general ill feeling may be present
- Headache
- Muscle soreness and joint aches
- And swollen lymph nodes
If the initial infection is not treated, the bacteria can spread throughout the body. Symptoms in this stage can be more widespread and severe, including:
- Multipe erythema migrans (EM) rashes
- Bell’s palsy (facial paralysis)
- Severe headaches, and neck stiffness
- Pain in joints, tendons, and muscles
- Heart palpitations, dizziness, irregular hearbeat
- Short-term memory problems and difficulty concentrating
- Fatigue may increase
- And neurological symptoms like shooting pains, numbness, or tingling in the hands and feet
In the most advanced stages, the infection can cause chronic, severe symptoms. This can manifest as:
- Chronic arthritis, often in the large joints like the knees
- Neuropathy
- Cognitive dysfunction
- Severe fatigue and general lack of stamine
- Neurological issues can also be more profound, leading to cognitive problems, memory issues, nerve damage, and extreme fatigue.
🧪 Lyme Disease Testing and Lyme Disease Diagnosis
Diagnosing Lyme disease can be challenging, since symptoms often differ between individuals and may resemble those of other illnesses. While blood tests are the most common tool to confirm the diagnosis, additional diagnostic methods may also be considered.
Current Lyme disease tests are often inaccurate, ranging between 20%-50% accuracy depending on the testing method. Because of these limitations, Lyme disease is often clinically diagnosed. If you suspect an infection, it is essential to consult a knowledgeable physician for proper testing and clinical diagnosis. Without proper treatment, Lyme disease can progress and become chronic, affecting multiple systems and leading to persistent symptoms.
It’s crucial to take signs of Lyme disease seriously, even if they aren’t always recognized or supported by doctors. If you suspect you may have Lyme disease, advocate for yourself and explore our resources on reliable testing.
💊 Lyme Disease Treatment
Early treatment of a Lyme disease infection is crucial to reduce the risk of complications. Managing the illness usually requires a combination of strategies aimed at relieving symptoms, controlling infection, and preventing long-term effects.
There is no standard single treatment for Lyme disease. Many patients must try different approaches -or a combination of them- before finding what works best.
Most common treatments include:
- A combination of oral or intravenous antibiotics
- Herbal protocols, or
- Alternative therapies.
🔗 Lyme Disease Co-Infections
Some patients experience long-term symptoms even after a standard course of antibiotics. This is known as Post-Treatment Lyme Disease Syndrome (PTLDS). It’s also sometimes referred to as chronic Lyme disease.
According to many Lyme-literate doctors, these lingering symptoms can have different reasons. First, the initial antibiotic course may not have been enough to eradicate the infection. Second, while the Lyme infection may have been cleared, a tick can transmit other pathogens in addition to Borrelia, leading to so-called co-infections and resulting in multiple infections. The most common co-infections of Lyme disease are:
- Anaplasmosis
- Babesiosis
- Bartonella
- Mycoplasma
- And sometimes viral infections such as Powasan virus.
These co-infections must be addressed to see a full clearance of symptoms.
⚡ Lyme Disease, Mast Cell Activation Syndrome (MCAS), and Histamine Intolerance (HIT)
Researchers estimate that mast cell activation syndrome (MCAS) affects up to 17% of the population. Syptoms of MCAS and histamine intolerance, such as food sensitivities and multiple chemical sensitivities, are often observed in people suffering from Lyme disease. If you have a history of these issues or a suspected MCAS diagnosis, it’s important to understand this connection. Treating Lyme without addressing a co-existing MCAS can make the healing process much more difficult and even stall progress.
🛡️ Prevention is better than cure!
Researchers estimate that mast cell activation syndrome (MCAS) affects up to 17% of the population. Syptoms of MCAS and histamine intolerance, such as food sensitivities and multiple chemical sensitivities, are often observed in people suffering from Lyme disease. If you have a history of these issues or a suspected MCAS diagnosis, it’s important to understand this connection. Treating Lyme without addressing a co-existing MCAS can make the healing process much more difficult and even stall progress.
🧭 Want a Simple Roadmap Through Lyme?
Lyme can feel overwhelming – symptoms, testing, treatments, lifestyle changes.
That’s why we created a FREE 5-Step Lyme Roadmap to guide you from the very first signs to practical next steps. A simple but powerful guide that brings everything into one place.
📩 Download your copy now!
